Throughout the last few years, we have seen the fallout from inequitable COVID-19 responses across the United States. This has reinvigorated dialogues about the intersections between health equity, public health, and nursing – particularly in remote, reservation-based communities.
It is well documented that Native Americans experienced a disproportionate burden of COVID-19, in infection rate, hospitalization rate, and in mortality rate. However, what was not highlighted in the media, was the federal government’s neglect of Native American communities at the height of the pandemic. Unfortunately, this comes as no surprise to many across Indian Country, given the government’s blatant disregard for numerous treaties and failure to provide necessary preventive medical treatment to curb pervasive health inequities.
Collectivist Approach to Public Health and Wellbeing
The inherent resilience and strength within the Native American communities are to be admired. Crystal Echo Hawk, founder and executive director of Illuminative, said that in response to COVID-19: “…folks began to organize in the Tribal communities. Tribal leadership stepped up. The average Tribal citizen stepped up and said we need to take care of our own.”
Public health nurses (PHNs) were front and center leading community-based, pandemic-related efforts and are integral to communities’ wellbeing at-large. Tribal PHNs were at the frontline in responding to COVID-19 as well as organizing and administering vaccines, resulting in Native Americans having the highest COVID-19 vaccination rate. The Indian Health Service (IHS) reported administration of just 2.3 million doses of the COVID-19 vaccine across IHS Service Units in the United States. As public health experts in their communities, PHNs also led efforts in contact tracing and provided valuable leadership in the emergency response efforts across Indian Country. Safeguarding the health of the community requires continuous surveillance and engagement with individuals, families, groups, and the entire community.
Aside from public health emergencies, PHNs have pivotal roles in school health nursing, supervising and supporting Community Health Representatives (CHRs), staffing specialty clinics, and coordinating transitions of care, equipment delivery, and home-based nursing care. Despite their extensive service and dedication to collective health and wellbeing, PHNs’ tireless efforts in remote Native American communities often go unrecognized and remain invisible to community and hospital leaders. Such invisibility can contribute to increased stress and burnout, and decreased engagement in the workplace.
The Public Health Nursing Workforce Shortage is Real
Despite growing acknowledgement of the need for PHNs, the workforce has remained largely stagnant for decades – particularly in rural and reservation-based communities. The formulas for IHS PHN staffing are census or user-based with nurse-to-patient ratios of 1.5 PHNs to ~1,250 patients – and unrealistic and unsustainable workload. Additionally, the scope and function of PHNs drastically vary by region and setting, making it difficult to sufficiently enumerate their impact.
The Public Health Workforce Taxonomy has been working diligently since 2014 to comprehensively capture classifications and job descriptions to develop a standardized process that accurately describes the word PHNs do, especially in rural and underserved areas. Collectively, nurses must advocate for professional organizations, such as the American Public Health Association, to prioritize clear definition and scope of the PHN role and movement towards standardized reporting, so that policymakers have sufficient data to justify legislation that will increase supply and enhance relevant workforce development programs.

Case Example: Community-Of-Practice to Support Public Health Nurses in Fort Belknap
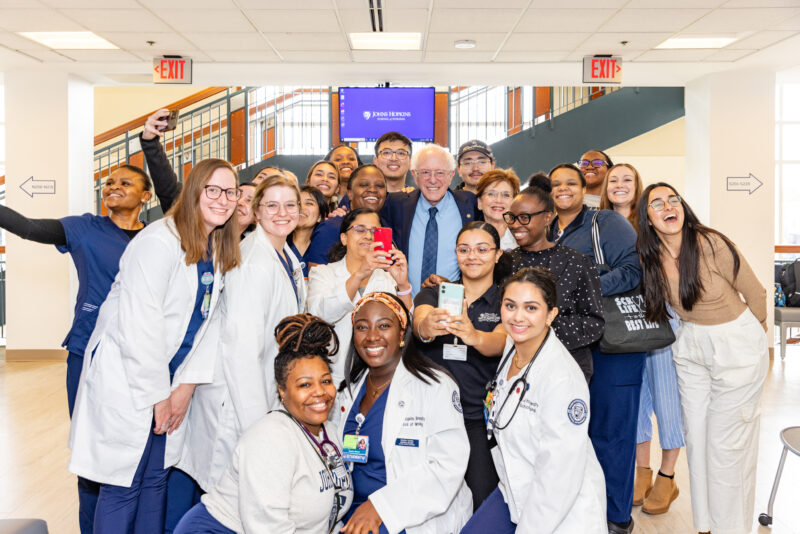
With guidance from Dr. Teresa Brockie, the Johns Hopkins University School of Nursing and the Fort Belknap Indian Community have taken steps to solidify their “research-practice partnership” – a community-driven avenue for achieving health equity. In light of barriers PHNs are experiencing, Dr. Brockie’s team has developed a Community of Practice (CoP) to promote the sharing of best-practices and ideas. Etienne Wenger-Trayner, a globally recognized thought leader, defined CoPs as “Groups of people who share a concern or a passion for something they do and learn how to do it better as they interact regularly”. With this framework in mind, both groups – and those with shares interests – come together to develop relevant education, training, and career advancement opportunities to enhance the capacity of this incredible all-Native American PHN team.
We welcome those with shared interests to join our CoP! If you are interested in getting involved, contact Research Program Coordinator, Mina Kazemi at [email protected].
About the Authors:

Katie Nelson, MSN, RN, is a PhD candidate at the Johns Hopkins School of Nursing. Her research focuses on principles of justice and equity in health care access and delivery among Native American patients, families, and communities in the context of serious illness.
Kathleen Adams, BSN, RN, is a Public Health Nurse and Manager in the Fort Belknap Tribal Health Department. She is a member of the A’aanii tribe at Fort Belknap Reservation. Her role as a Public Health Nurse is to promote wellness, prevent illness, and protect the health of the community as a whole.


Michelle Kahn-John, PhD, RN, PMHNP-BC, GNP, is a Research Associate at the Johns Hopkins School of Nursing. She is a member of the Navajo Nation, Big Water Clan. Her research leverages the Navajo concept of Hózhó, a wellness philosophy and belief system, focusing on the relationship between cultural practices and physical and psychological health of Indigenous populations.
Teresa Brockie, PhD, RN, FAAN, is an Assistant Professor at the Johns Hopkins School of Nursing and has a joint appointment in the Johns Hopkins Bloomberg School of Public Health Center for Indigenous Health. She is a member of the White Clay Nation (A’aninin) from the Fort Belknap Reservation. Her research focuses on achieving health equity through community-based prevention and intervention of suicide, trauma, and adverse childhood experiences among vulnerable, reservation-based populations.

More from On The Pulse: